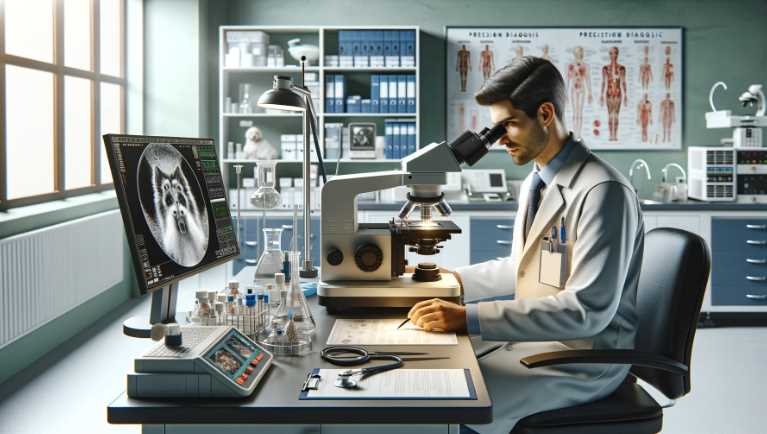
Microscopic Marvels: How Veterinary Microscopes Revolutionize Animal Healthcare
Veterinary personnel is often required to inspect animals for injuries, illnesses, or abnormalities. A microscope is an essential tool for these professionals for two main reasons: First, it allows them to see details that would otherwise be invisible to the human eye. Second, it can be used to determine the cause of an injury or […]
Microscopic Marvels: How Veterinary Microscopes Revolutionize Animal Healthcare Read More »