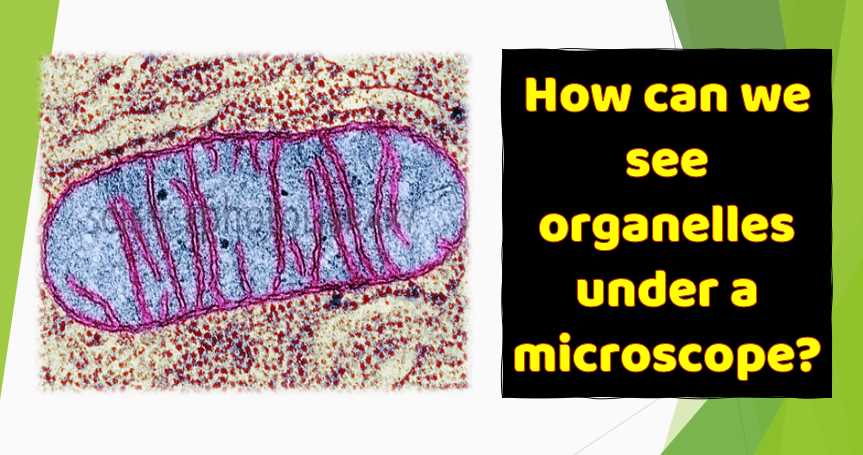
Chlamydia is a bacteria that cannot be seen with the naked eye. Under a microscope, Chlamydia appears as small, round, or oval-shaped cells.
Chlamydia trachomatis is an obligate intracellular bacterium, meaning it can only survive and replicate inside host cells. When observed under a microscope, Chlamydia cells typically appear as small, gram-negative, cocci or rod-shaped structures. However, the exact appearance can vary depending on the stage of the chlamydial life cycle.
Chlamydia has a unique developmental cycle involving two forms: the infectious elementary body (EB) and the replicative reticulate body (RB). The elementary body is the infective form, while the reticulate body is responsible for replication. These forms can be distinguished under a microscope based on their size and morphology.
| Aspect | Characteristics |
|---|---|
| Size | Approximately 0.2 to 1.5 micrometers in diameter |
| Shape | Can appear as cocci or rod-shaped structures |
| Staining | Gram-negative |
| Life Cycle | Two forms: Elementary Body (EB) and Reticulate Body (RB) |
| Infectious Stage | Elementary Body (smaller, more compact) |
| Replicative Stage | Reticulate Body (larger, less compact) |
| Intracellular Growth | Obligate intracellular bacterium |
The Basics of Chlamydia
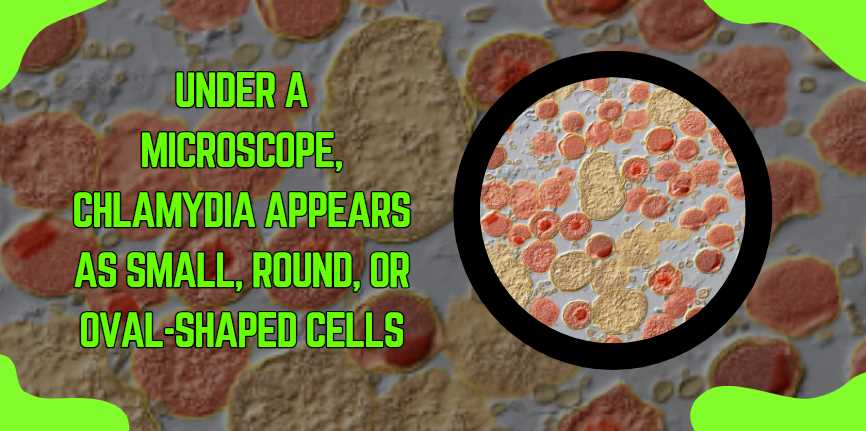
Chlamydia is a common sexually transmitted disease (STD) caused by the bacterium Chlamydia trachomatis. It can infect both men and women, and leads to serious reproductive and other health problems if left untreated. One of the key methods used by scientists to understand and diagnose Chlamydia is through microscopic examination. But, what does Chlamydia look like under a microscope? Let’s explore the unique visual characteristics of this bacterium.
Observing Chlamydia Under the Microscope
When examining Chlamydia under a microscope, there are several stages and morphological forms you may observe:
Elementary Bodies (ebs)
The infectious form of Chlamydia is known as elementary bodies (EBs). Under a high-powered microscope, EBs appear as tiny, dense, spherical particles. They are small, typically around 0.2 to 0.3 micrometers in diameter. Because of their size and shape, they can sometimes be mistaken for viruses.
Reticulate Bodies (rbs)
Reticulate bodies (RBs) are the non-infectious, replicative form of Chlamydia. They are larger than EBs, roughly 1 micrometer in diameter, and less dense. RBs are observed within the host cell’s inclusion bodies, which are essentially membrane-bound vacuoles utilized by the bacteria for replication.
Inclusion Bodies
Inclusion bodies are a hallmark of Chlamydial infection. They are formed within infected eukaryotic cells and consist of a mass of reticulate bodies and elementary bodies. Under light microscopy, these inclusions appear as irregularly shaped, larger structures within the host cell.
| Form | Appearance under Microscope | Diameter | Location |
|---|---|---|---|
| Elementary Bodies (EBs) | Dense, spherical particles | 0.2 – 0.3 µm | Outside host cells, infectious |
| Reticulate Bodies (RBs) | Less dense, larger than EBs | About 1 µm | Within inclusion bodies, non-infectious |
| Inclusion Bodies | Irregularly shaped, large structures | Varies | Inside host cells |
Staining Techniques to Visualize Chlamydia
In order to properly visualize Chlamydia under a microscope, various staining techniques are used. The most common staining technique is the Giemsa stain, which colors the inclusions formed by the bacteria, making them more visible against the background of host cells. The immunofluorescence technique can also be used, where fluorescent dyes are attached to antibodies that specifically bind to Chlamydia, resulting in brightly colored inclusions under fluorescent microscopy.
How is Chlamydia Diagnosed Microscopically?
Microscopic Diagnosis:
Diagnosing Chlamydia microscopically involves examining samples collected from the infected site under a microscope. The most common method is staining the samples using specific techniques.
| Method | Description |
|---|---|
| Direct Immunofluorescence (DFA-IF) | Uses fluorescent antibodies to detect Chlamydia |
| Nucleic Acid Amplification Tests (NAAT) | Detects Chlamydia DNA for high sensitivity |
Sample Collection:
Samples for microscopic diagnosis are typically collected from the infected site, such as the cervix, urethra, or rectum. In women, a cervical swab is commonly used, while men may undergo a urethral swab. These samples are then processed for microscopic examination.
| Sample Type | Collection Site |
|---|---|
| Cervical Swab (Women) | Cervix |
| Urethral Swab (Men) | Urethra |
| Rectal Swab | Rectum |
Microscopic Examination:
The collected samples are examined under a microscope after appropriate staining. Direct Immunofluorescence (DFA-IF) involves using fluorescent antibodies that specifically bind to Chlamydia antigens, making the bacteria visible under fluorescence microscopy. Nucleic Acid Amplification Tests (NAAT) detect Chlamydia DNA, providing a highly sensitive and specific diagnostic approach.
| Technique | Advantages |
|---|---|
| DFA-IF | Rapid, specific, and visual confirmation |
| NAAT | High sensitivity; detects Chlamydia DNA |
Limitations:
While microscopic diagnosis is valuable, it may have limitations, such as potential false negatives. Sensitivity can vary, and the timing of sample collection in relation to infection can impact results. It’s essential to consider these factors when interpreting microscopic findings.
In conclusion, microscopic diagnosis of Chlamydia involves examining stained samples collected from the infected site. Techniques like Direct Immunofluorescence (DFA-IF) and Nucleic Acid Amplification Tests (NAAT) enhance the accuracy of Chlamydia detection under a microscope. If you suspect a Chlamydia infection, consult a healthcare professional for appropriate testing and guidance.
How Effective are Antibiotics in Treating Chlamydia?
Antibiotic Treatment:
Chlamydia is typically treated with antibiotics, and the choice of antibiotic depends on factors such as the patient’s health, allergies, and the presence of coinfections.
| Antibiotic | Treatment Duration |
|---|---|
| Azithromycin | Single oral dose |
| Doxycycline | Twice daily for seven days |
Efficacy:
Both Azithromycin and Doxycycline are highly effective in treating Chlamydia. They work by inhibiting the growth and replication of the bacteria, ultimately clearing the infection. It’s crucial to complete the full course of antibiotics as prescribed by a healthcare professional to ensure complete eradication of the bacteria.
| Antibiotic | Mechanism of Action |
|---|---|
| Azithromycin | Inhibits bacterial protein synthesis |
| Doxycycline | Inhibits bacterial protein synthesis |
Follow-up Testing:
After completing the antibiotic treatment, follow-up testing is recommended to confirm the eradication of the infection. This ensures that the antibiotics were effective and that there is no lingering Chlamydia presence.
| Follow-up Testing | Purpose |
|---|---|
| Nucleic Acid Amplification | Confirms eradication of Chlamydia |
Preventing Re-infection:
To prevent re-infection, individuals treated for Chlamydia should abstain from sexual activity until the full course of antibiotics is completed. Additionally, notifying and treating sexual partners is essential to prevent the spread of the infection.
Recap
Understanding what Chlamydia looks like under the microscope is crucial for its diagnosis and treatment. It allows healthcare professionals to identify the presence of the bacteria and to discriminate between Chlamydia and other STDs with similar symptoms. Microscopic analysis is an essential tool in the arsenal of medical microbiology for both research and clinical diagnostics.

Fahim Foysal is a well-known expert in the field of binoculars, with a passion for exploring the great outdoors and observing nature up close. With years of experience in the field, Fahim has honed his skills as a binocular user and has become a go-to resource for those seeking advice on choosing the right binoculars for their needs.
Fahim’s love for the natural world began during his time at The Millennium Stars School and College and BIAM Laboratory School, where he spent much of his free time exploring the outdoors and observing the wildlife around him. This passion for nature led him to pursue a degree in Fine Arts from the University of Dhaka, where he gained a deep understanding of the importance of observation and attention to detail.
Throughout his career, Fahim has used his expertise in binoculars to help others discover the beauty of the natural world. His extensive knowledge of binocular technology and optics has made him a trusted advisor for amateur and professional wildlife observers alike. Whether you’re looking to spot rare birds or observe animals in their natural habitats, Fahim can help you choose the perfect binoculars for your needs. With his guidance, you’ll be able to explore the outdoors with a newfound appreciation for the beauty of the natural world.
Table of Contents